There are many large research studies available on treatment of hemifacial spasms by micro vascular decompression surgery. Considering the rapid improvements in the neurosurgical instrumentation, neuro-microscopes, neuro-anaesthesia and neuro-intensive-care, the results of these surgeries have remarkably improved in last few years and hence it would be prudent to refer to a large series done only after the year 2000.
One such series is summarised here, in a paper written by Hyun S J, Kong DS & Park K in 2010 July issue of Neurosurgery Review. It describes 1174 patients operated between 1997 and 2009. Out of 1174 patients, 1105 patients (that is 94.1% patients) were totally ‘cured’ (no spasms) and out of the remaining 5.9% patients, majority had good outcome with only few residual spasms.
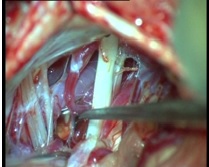
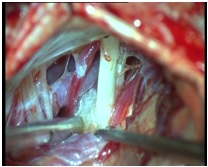
In our personal series of 67 patients, operated between the year 2010 to 2014 by a single neurosurgeon ( Dr. Jaydev Panchawagh) with almost the same assisting and anaesthesiologist’s team, 99% had complete relief ( follow up 7 months to 4 years) and 1% had remarkably improved status.
Majority of the large series reported before 2010, including that of Dr. Peter Jannetta, have emphasized that the success of Micro-Vascular Decompression surgery for hemifacial spasms tends to be long lasting and recurrence is rare. Complications are rare including transient facial paresis and transient hearing loss in 1 to 2 % of patients, and extremely rare incidence of permanent deficits. In short, Micro-Vascular Decompression for facial twitching in a modern-facility neurosurgical centre is a reasonably safe, effective and dramatic surgery; it has the potential to cure hemifacial spasms.